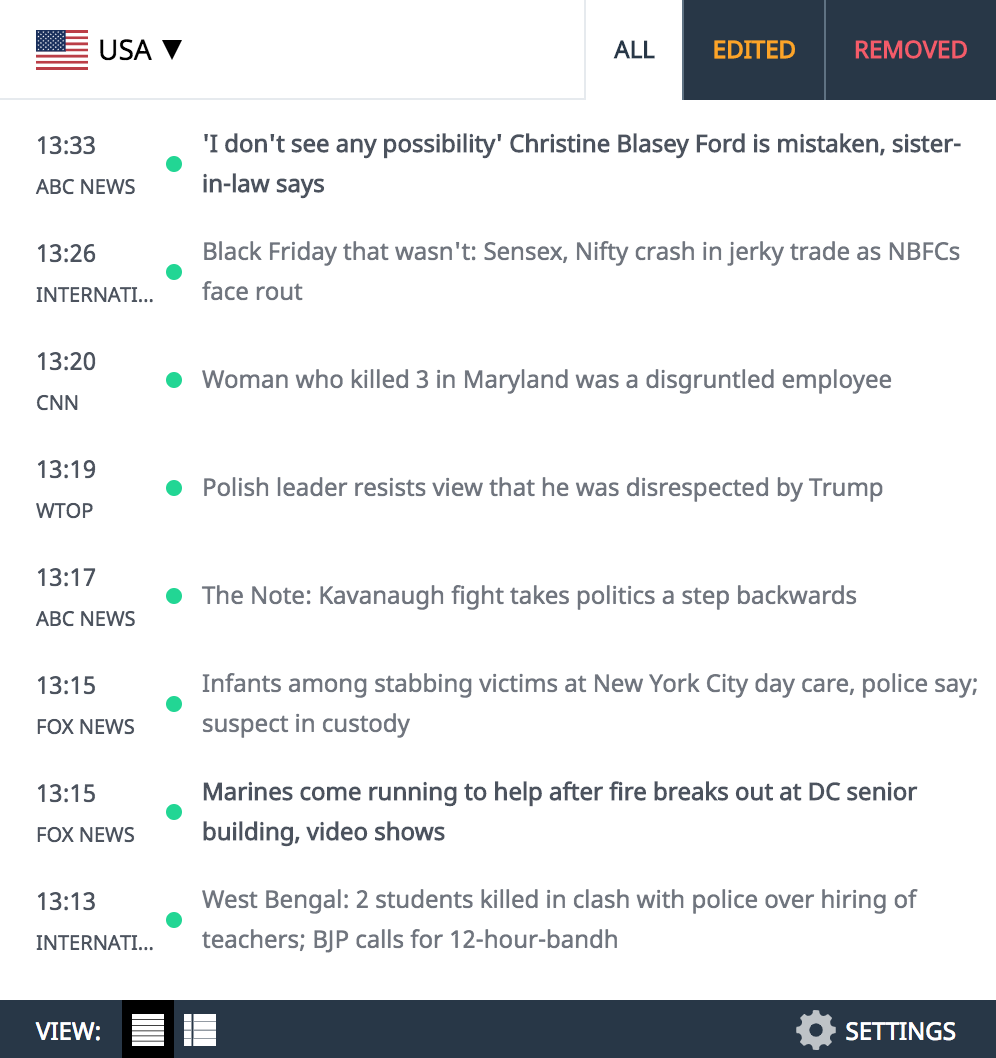
Researchers at Johns Hopkins Medicine have reported that, in a small study of adults with major depression, administration of two doses of the hallucinogenic drug psilocybin, with supportive psychotherapy, produced large and rapid reductions in depressive symptoms. Most of the participants showed improvement, and half of those who participated in the study had remission through the four weeks of follow-up.
Psilocybin, a substance found in so-called “hallucinogenic mushrooms,” produces visual and auditory hallucinations and profound alterations in consciousness within a few hours of being ingested. In 2016, Johns Hopkins Medicine researchers were the first to find that psilocybin treatment in conjunction with psychological support reduced existential anxiety and depression in people diagnosed with life-threatening cancer.
TIP: Get our latest content by joining our newsletter. Don't miss out on news that matter in Costa Rica. Click here.
Effective in the much larger population of patients
Now, the results of the new study, published Nov. 4 in JAMA Psychiatry, hint that psilocybin might be effective in the much larger population of patients with major depression than previously appreciated.
“The magnitude of the effect we saw was nearly four times greater than what clinical studies have shown using conventional antidepressants on the market,” says Alan Davis, Ph.D., associate professor of psychiatry and behavioral sciences in the School of Medicine. from Johns Hopkins University. “Since most other depression treatments take weeks or months to work and can have undesirable effects, this could be a game changer, if these results are supported by future placebo-controlled clinical trials that are the gold standard. reference”. The published results cover only a four-week follow-up of 24 participants, all of whom received two 5-hour sessions of psilocybin under the direction of the researchers.
“Because there are different types of major depressive disorder that can cause variations in how people respond to treatment, I was surprised that nearly all of the participants in our study found psilocybin treatment effective,” says Roland Griffiths, Ph.D., Oliver Lee McCabe III Professor of Neuropsychopharmacology and Consciousness at Johns Hopkins University School of Medicine and director of the Johns Hopkins Center for Research in Psychedelic Experience and Consciousness (Johns Hopkins Center for Psychedelic and Consciousness Research).
He notes that the major depression treated in the new study may have been different from the ‘reactive’ form of depression in the patients they included in the cancer clinical trial in 2016. Dr. Griffiths notes that public health officials urged his team to explore the effects of psilocybin in the broader population of those with major depressive disorder because of the much larger impact it could have on public health.
The new study
For the new study, scientists recruited 24 people with a documented history of long-term depression, most of whom had had persistent symptoms for about two years before enrolling in the study. The average age of the participants was 39 years; 16 were women and 22 identified as white, one person as Asian, and one person as African American. Participants had to gradually stop taking their antidepressants before the study, with the support of their treating physician, to ensure safe exposure to this experimental treatment.
Thirteen participants received the psilocybin treatment immediately after recruitment and preparatory sessions, and 11 participants received the same preparation and treatment after an eight-week delay.
The treatment consisted of two doses of psilocybin administered by two clinical supervisors who provided guidance and support. It took place at the Johns Hopkins Bayview Behavioral Biology Research Building, two weeks apart, between August 2017 and April 2019. Each treatment session lasted approximately five hours, with the participant lying on a sofa, with a wearing a mask and headphones that played music and with the supervisors present.

All participants were given the GRID-Hamilton Depression Rating Scale (a standard method for assessing depression) at enrollment, and also at one and four weeks after completing treatment. On this scale, a score of 24 or more indicates severe depression, 17 to 23 moderate depression, 8 to 16 mild depression, and 7 or less no depression. At enrollment, participants had an average score of 23 on the Depression Rating Scale, but after one week and after four weeks of ending treatment, participants had an average score of eight on the Depression Rating Scale. for evaluation of depression.
Significant reduction in their symptoms
After treatment, most participants had a significant reduction in their symptoms, and almost half had remission of depression at the follow-up appointment. Participants in the delayed condition reported no reduction in their symptoms before receiving psilocybin treatment.
Of the group of 24 participants in total, 67% had a reduction of more than 50% in depression symptoms at the follow-up appointment one week later, and 71% at the follow-up four weeks later. Overall, at four weeks after treatment, 54% of the participants were considered to be in remission—meaning they no longer met the criteria for being depressed. The researchers say they will follow the participants for a year afterward to determine how long the effects of psilocybin therapy last.
Dr. Griffiths, who began his research with psilocybin in the early 2000s and was initially viewed with skepticism and concern by some, says he is pleased to have the support of Johns Hopkins and is encouraged to see the dozens of new businesses and research laboratories that have followed suit by doing their own research. He adds that a large number of companies are currently actively involved in developing marketable forms of psilocybin and related hallucinogenic substances.
According to data provided by the National Institute of Mental Health, more than 17 million people in the United States and 300 million people worldwide have had symptoms of major depression.
LIKE THIS ARTICLE? Sign up to our newsletter and we will send you updates of our latest content as soon as they are available. Click here.