Level Zero is related, in part, to a logjam of ambulances delayed while waiting to offload patients at busy hospitals and has become more common during the pandemic

There were no ambulances available in Ottawa on the October day a frantic 911 call came in from an elementary school about an 11-year-old girl who had no vital signs, the head of Ottawa’s paramedic service has confirmed.
Acting Chief Peter Kelly said in a statement that the Ottawa Paramedic Service was at Level Zero, meaning no ambulances were available to immediately respond, when the call came in during the early afternoon on Oct. 25. It was a Code 4 — the highest priority for paramedic response in the city
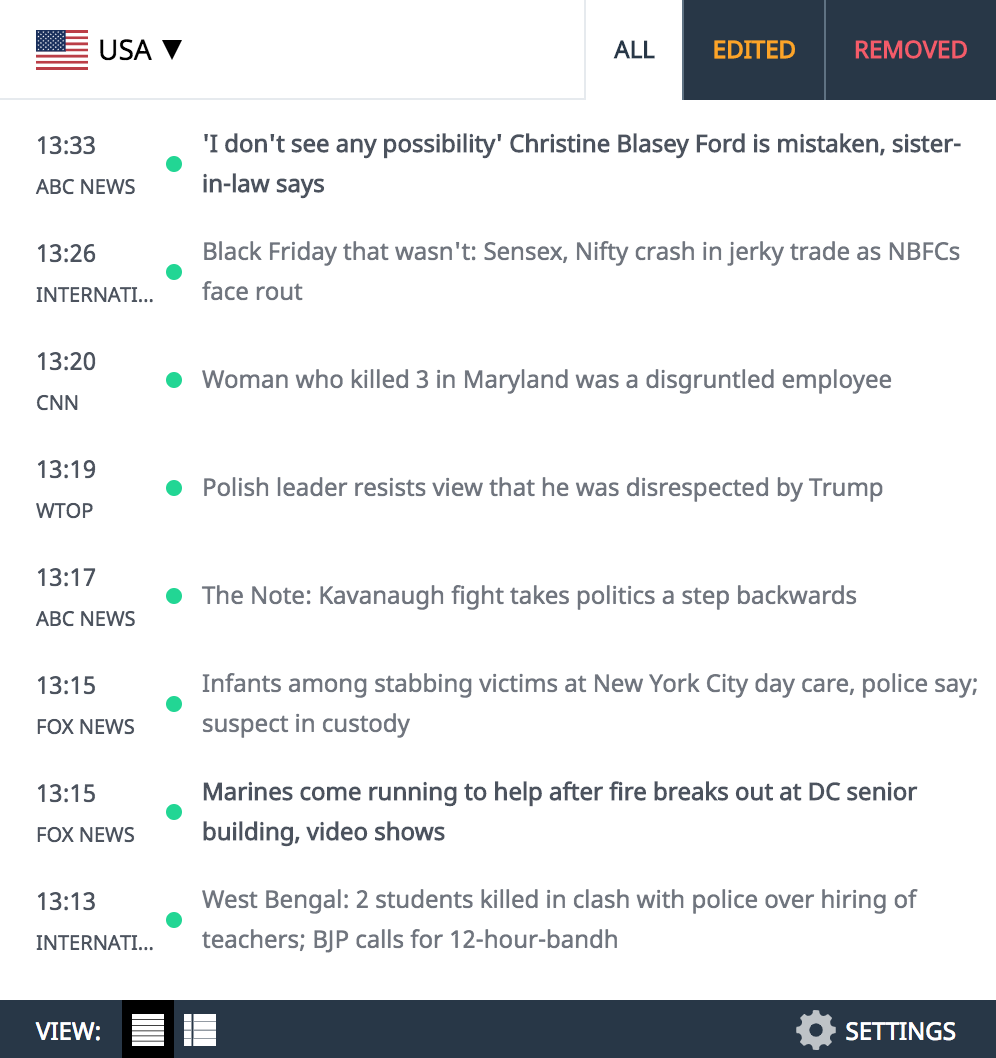
Sign up to receive daily headline news from Ottawa Citizen, a division of Postmedia Network Inc.
Thanks for signing up!
A welcome email is on its way. If you don't see it, please check your junk folder.
The next issue of Ottawa Citizen Headline News will soon be in your inbox.
Level Zero has been a growing crisis in Ottawa and across the province in recent years. It is related, in part, to a logjam of ambulances delayed while waiting to offload patients at busy hospitals and has worsened during the pandemic. There are expected to have been well over 1,000 periods of Level Zero in the city by the end of the year, with a projected 60,000 hours of offload delays for paramedics.
People at the school performed CPR on the girl until help arrived. A bystander was able to use the school’s public-access defibrillator within four minutes of the 911 call, according to a statement from the City of Ottawa.
The girl, who had cerebral palsy and relied on a wheelchair, was pronounced dead after being transported to CHEO. The regional coroner’s office is investigating her death.
The girl’s family declined to comment, but a spokesperson said they did not have concerns about the response to her medical crisis.
“CPR was initiated immediately. That is what is important.”
Initially, help came from the Ottawa Fire Service. Paramedics arrived later, including at least one who had just signed off work and was alarmed about the unfolding situation, according to a source familiar with the case who asked to remain anonymous because they were not authorized to speak about the situation.
Firefighters arrived on the scene four minutes after being assigned the call, according to a statement from Kelly, and continued to treat the girl. Paramedics, who carry and are trained to administer cardiac medication as well as equipment to intubate patients, arrived 11 minutes later to treat and transport the girl to CHEO.
The provincial target for response times to 911 calls for sudden cardiac arrest is six minutes.
Targeted sudden cardiac arrest response time is considered to be met “if a public access defibrillator is available at the scene or by the arrival of a paramedic, police officer, firefighter or OC Transpo Security, who are all equipped with a defibrillator in their vehicles,” Kelly said in an emailed statement.
“The Ottawa Paramedic Service was experiencing Level Zero during the time of this call. In these instances, the service mitigates its offload delays and incidences of level zero by implementing existing measures with the support of Ottawa Fire Services and other paramedic services to meet the demand for service,” Kelly said.
A paramedic response unit was dispatched to the scene from an unknown distance, according to the source.
Kelly said the Ottawa Paramedic Service “along with other paramedic services across Canada, continues to experience unprecedented service impacts” as a result of the ongoing system-wide health-care crisis across the country.
“Offload delays incurred at hospitals, along with consistently high call volumes, has put an extra strain on our resources and remain a significant contributor to level zero incidences.”
In August, then-mayor Jim Watson asked the province to fund 42 new paramedic jobs in Ottawa to help the city reduce level zero incidents.
He said the new paramedics would be stationed at four Ottawa hospitals to care for lower acuity patients and allow ambulances to get back on the road more quickly.
“We can’t allow this to go on. We need the provincial government’s help. Health care is a provincial responsibility,” Watson said in his letter to Premier Doug Ford.
There has been no direct public response from the province to that request. A spokesperson for the Ministry of Health said it is working with paramedic services, hospital leadership and other sector partners “to increase ambulance availability and reduce ambulance offload time so all Ontarians will have access to the care they need, when they need it.”
Ministry of Health spokesperson Bill Campbell said the province has a strategy to tackle ambulance offload time, improve patient flow and avoid unnecessary trips to the emergency departments that includes $1.5 million to be spent in Ottawa for a dedicated offload nursing program that allows paramedics to get back on the roads.
Campbell also offered “our sincere condolences to this family over their tragic, sudden loss.”
A source familiar with the case says a better ambulance 911 triage tool — one many municipalities and paramedics have been requesting for years and a handful of Ontario municipalities are using — could make a difference in cases of sudden cardiac arrest, even when there are few ambulances available.
There are two ambulance call triage tools used in Ontario ambulance communications centres. Ottawa, along with the vast majority of municipalities, uses the Dispatch Priority Card Index. A few municipalities use the Advanced Medical Priority Dispatch System, which is widely used around North America and which does a better job of prioritizing calls, including those for sudden cardiac arrest in which minutes can make the difference between life and death.
An anonymous Ottawa social media account that tracks incidents of Level Zero in the city had tweeted details of the case involving the young girl in October, including that at least one off-duty and reassigned paramedic, aware of the unfolding situation, formed part of the team that treated and transported the girl to hospital. Paramedics were able to restore her pulse but she was pronounced dead at the hospital.
The Twitter account said some paramedics, aware of the situation, rushed to offload patients and clean their equipment, only to be sent to other Code 4 calls waiting in the queue that included a fall and an unknown situation. Under the system used in Ottawa and elsewhere, a variety of calls are given the highest priority. Once an ambulance is assigned to a Code 4, it cannot be diverted by the dispatcher to another call unless another ambulance can get there quicker, according to a briefing on the system prepared by the Regional Municipality of Hamilton.
“Under the current prioritization system from the Ministry of Health, all Code Four calls are assigned in the order they are received to the closest available paramedic unit. Code Four calls are those where the patient is in life-threatening or in immediate danger,” Kelly said in an emailed statement.
A coroner’s inquest into the death of Greely resident Alice Martin of heart failure back in 2004 found that paramedics were not responding to patients fast enough, and recommended that Ottawa implement the Advanced Medical Priority Dispatch system, which the coroner’s report called “far superior” to the existing Ottawa system.
In the case of the young girl, her obituary said she handled many health challenges with “admirable courage, strength, grace, and faith” and invited those wishing to donate to do so to CHEO or the Muscular Dystrophy Association.