A teenager in Vancouver with severe epilepsy wears a life-saving device in his brain to reduce seizures. This is an American procedure that is not yet available in Canada.

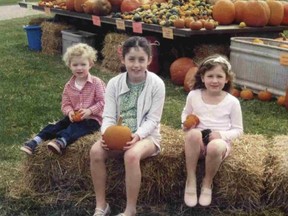
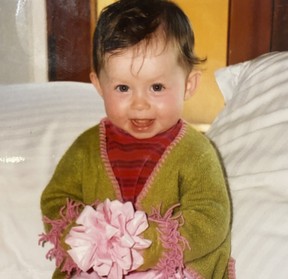
As a young girl, Sophie Corwin He loved painting, was intrigued by mythology, and dreamed of becoming a marine biologist one day to study underwater creatures.
She is a typical childhood and she is "very tasty, nice and easy" until her mother changed everything at the age of eight without warning. It states.
"I was just listening to music," recalls Sophie, now 20. "And I was in a coma."
Her mother, Catherine Corwin, first found her. "Her eyes were rolling backwards in her head. She was almost purple. She was unconscious. And she had a large puddle of vomit next to her.
"In the ambulance, Sophie was so bad that she couldn't drip and wasn't breathing."
She was in a coma for 17 hours. When she woke up, it was for a very different future.
She needed 18 months of medical examination before she was finally diagnosed after that horrifying day in October 2009. Sophie suffered from severe epilepsy. Her seizures were not accompanied by convulsions, but typically included vomiting, loss of speech, very low body temperature, and often loss of consciousness.
Doctors will also discover that she is resistant to the drug. This means that there is no medicine that can be taken to control her seizures. Her seizures lasted for hours and she became more and more life-threatening.
By 9th grade, this vibrant and curious child was no longer able to attend school. Instead of going to art lessons or swimming, she spent too many days in the hospital either recovering from a catastrophic seizure or taking a test of possible solutions.
All the doors her Vancouver parents tried to open-visiting two specialty hospitals in the United States and extensive genomic sequencing looking for genetic clues-closed without an answer.
Sophie was not even a candidate for epilepsy-related surgery in Canada because of the area of the brain where seizures are occurring. The family learned of nasty news in 2017 after being tested at a university hospital in London, Ontario. There, experts inserted 25 electrodes deep into the brain to determine the cause of the seizure.
But a London doctor tells his family about a state-of-the-art deviceresponsive neurostimulation therapy(RNS) that was approved just three years ago. did. USA —But it wasn't offered in Canada. This includes inserting a device approximately the size of a thick credit card into Sophie's brain to detect and suppress seizures before they occur.
Cowin consulted a New York doctor, but Sophie, who was initially 16 years old, wasn't very keen on putting the device in her head.
"I didn't like it. It took me a while to accept it. I felt like a cyborg," Sophie said in a serious conversation with her friendly sense of humor. I said while blinking.
However, with few options, her family made the difficult choice of proceeding with an invasive procedure.
"This is still a new technology, but I have no other choice. I ran Plans B, C, D, E, F, G. That's it. And it wasn't sustainable to continue living like this. You can survive no matter how many times you're in the intensive care unit, "Catherine said.
"I think she was the first patient to wear RNS in Canada at the time of Sophie's surgery in November 2017."

This device reduces the effects of Sophie's seizures and makes a visit to her hospital. I reduced it, but she hasn't healed. Her epilepsy and her daily activities are still very limited. But she believes Catherine was an opportunity to save her daughter's life.
The difficult decisions faced by Cowin and three other Canadian families with children with drug-tolerant epilepsy will be premiered this Wednesday in a new documentarySeizingHope {108. } Is the focus. Vancouver's Van City Theater.
There are about 600,000 children with epilepsy in North America, of which about one-third do not stop seizures.
One of the key goals of the documentary is to give hope to these families, said Dr. Judy Iles of the University of British Columbia. Professor of Neurology and co-executive producer of documentaries. "A new kind of technique for the brain may really be able to improve this type of epilepsy that is resistant to medication," she said. The
documentary is the result of a four-year study of ethics on pediatric epilepsy, neurotechnological options for patients, and invasive brain surgery by members of the UBC'sNeuroethics Canadagroup. ..
We are exploring "the importance of considering not only the technology itself, but the ethical implications of inserting electrodes into the child's brain, for example."
"The equation is always: Does the benefit outweigh the risk?"
The advantage is that these patients are ideally more social. She said it would be autonomous and reduce their stigma. These brain surgeries may not always be "silver bullets," but in the most severe cases, they can significantly improve survival, Illes said.
There are several types of brain surgery for children with epilepsy in Canada, but Iles says it is unacceptable that surgery performed by Sophie is only available south of the border.
"Why Canadians don't have access to the same advanced techniques as Americans. We need to catch up. We have to. We won't be left behind," she said. ..

Health Canada is considering introducing RNS technology to the country by the federal government. He has not received an application from the manufacturer, he just said, "Therefore, this medical device is not licensed for sale in Canada."
Therefore, epilepsy patients with similar problems to Sophie cannot undergo this life-saving surgery without cash to pay a large amount of US medical expenses. ..
Near-Death Seizures
Cowin reveals that drastic measures need to be taken to save Sophie, who had a near-dead seizure in 2014. became. , Lasted for 60 hours.
"Sophie held her breath and kept her life in the intensive care unit," said former intensive care nurse Catherine.
Subsequent seizures got worse. During one of them she couldn't swallow and she had to learn how to feed herself again.
So Sophie was overwhelmed by her idea of putting the device in her head in New York, but she "come" to the need to try it.
Her device is similar to a defibrillator that is implanted in the heart and sends an electric shock to restore the heartbeat, said the director of neurosurgery at the University of Manitoba. And the related professor, Dr. Patrick McDonald, explained. At UBC.
RNS detects that a seizure is occurring and stimulates another area of the brain to stop or prevent the seizure from spreading.
Traditionally, neurosurgery for epilepsy has been fairly "coarse," says McDonald's. The surgeon cuts out the part of the brain that causes the seizure. This is a procedure that can often affect the patient's memory.
It is "more elegant" to create a device that can control seizures instead. But something like Sophie, for example, could be further improved by making it smaller so that it doesn't stick out of the patient's skull, he added.
In addition, doctors have opened Sophie's skull twice more since the surgery in 2017. "Modified" surgery to turn on another electrode in the brain and battery replacement. In-device — This should happen every 3 years. She also uses the machine every day to download the data collected by the device and send it to a Seattle doctor. Your doctor will see you directly every three months.

Life and Death Matters
Provides this kind of insight The experience of three other young people in the documentary who had different forms of brain surgery would hopefully help families of children with drug-resistant epilepsy, says McDonald, co-executive producer of the film. I did.
"The balance between risk and benefit varies from person to person and from family to family. It also depends a little on the extent of the effects of the seizures. And Sophie is severely affected by them, which is life-threatening. We know it was becoming involved, "he said.
"If the outcome of doing nothing is higher, I think families and patients are more likely to accept the higher risk, and the potential benefits are important. So I think it's a difficult decision for any family. I think it was hard for Sophie's family to make, but in a way they felt this was their only hope.
"And, thankfully, it helped Sophie."
Since the surgery, Sophie's attacks have been less severe and she has had far fewer visits to the intensive care unit. , Recovery time is greatly reduced. "It gives me more freedom. I stopped going to the hospital (as much)," she said.
However, her "freedom" is limited. She is still mostly trapped in her home and one of her family members must always help with her when she has a seizure that often accompanies vomiting and the need for sleep. not.
She can take a three-hour online Emily Carr drawing course once a week, but by the time she's done she's completely exhausted I am. She also struggles to find her words as a result of so many seizures that affect her brain, and her stamina remains low.
"Epilepsy robbed her a lot. From middle school to middle school to high school, there are all the options to go to school," Catherine said. "Any option to get a job or live independently."
But for now, her family is grateful for the improvements she has made since her surgery and their I hope the story gives hope to others.
"As a family, epilepsy taught us perspective," Catherine said. "Nothing is important other than making sure Sophie is still with us. The other two kids all deal with ongoing concerns about what the day will bring about Sophie's survival. Get the care you need to do. "
lculbert @ postmedia. com

To receive daily headline news from Vancouver Postmedia Network Inc to sign up. Click the sign-up button to click the Sun
Thank you for registering.
A welcome email has been sent. If you don't see it, check your junk folder.
The next issue of Vancouver Sun Headline News will arrive in your inbox shortly.