U.S. Slashes Medicare Drug Prices: Januvia Sees 79% Cut in Historic Move
U.S. announces final prices for first-ever Medicare drug negotiation, affecting 10 costly medications. Merck's Januvia faces steepest cut at 79%, impacting 66 million beneficiaries.
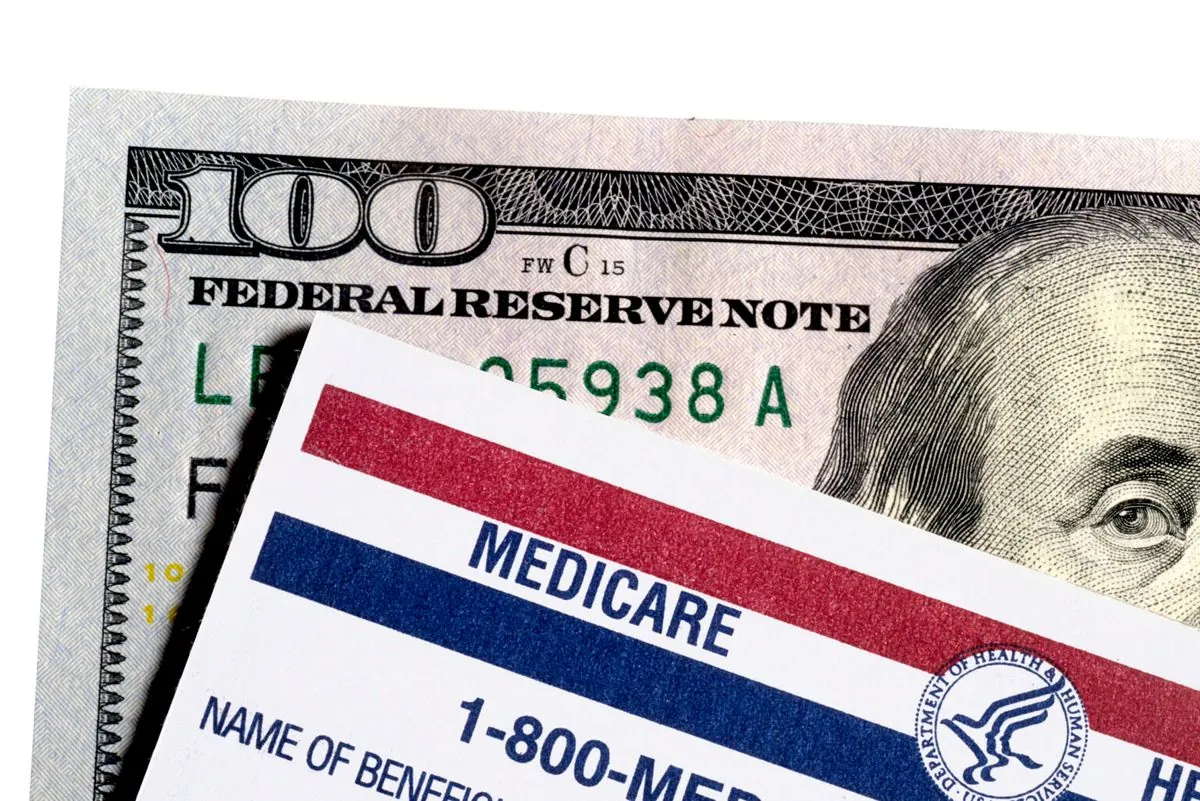
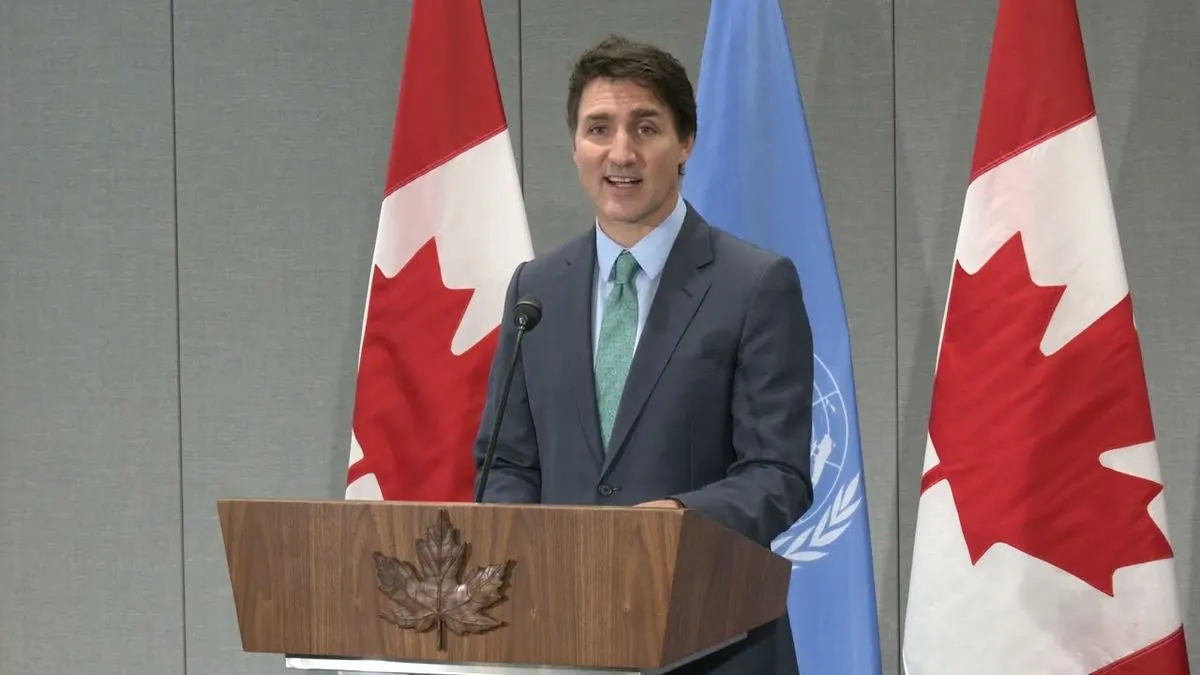
In a landmark decision, the United States government has revealed the final prices resulting from its inaugural negotiation of prescription drug costs for the Medicare program. This historic move, announced on August 15, 2023, targets ten of the most expensive medications covered by Medicare, a program serving approximately 66 million Americans aged 65 and older or with disabilities.
The negotiation process, made possible by the Inflation Reduction Act of 2022, marks a significant shift in U.S. healthcare policy. For decades, Medicare was prohibited from directly negotiating drug prices with pharmaceutical companies. This change aims to address the rising costs of prescription drugs in the United States, which has the highest per capita spending on pharmaceuticals among OECD countries, at $1,126 in 2021.
Among the negotiated drugs, Merck & Co.'s diabetes medication Januvia experienced the most substantial price reduction, with a 79% decrease. Januvia, first approved by the FDA in 2006, is a DPP-4 inhibitor used to treat type 2 diabetes. This significant price cut could have far-reaching implications for the global diabetes drugs market, which was valued at $61.87 billion in 2022.
Other medications affected by the negotiations include the popular blood thinner Eliquis, jointly marketed by Bristol Myers Squibb and Pfizer. Eliquis, approved by the FDA in 2012 for stroke prevention in patients with atrial fibrillation, has become a crucial medication for many Medicare beneficiaries.

The impact of these price reductions extends beyond individual drugs. The U.S. pharmaceutical market, which accounts for about 45% of the global market, may see significant changes in revenue and pricing strategies. This negotiation process could potentially influence the industry's approach to research and development, an area where pharmaceuticals outspend all other U.S. industries.
For Medicare beneficiaries, who on average spend about $1,300 per year on prescription drugs, these price reductions could lead to substantial savings and improved access to essential medications. The negotiation's effects may extend to the broader U.S. healthcare system, potentially influencing pricing for private insurance plans and out-of-pocket costs for patients.
As the U.S. FDA approves an average of 40-50 new drugs each year, the long-term implications of this negotiation process on drug development and approval remain to be seen. The balance between cost reduction and maintaining incentives for innovation will likely be a key consideration in future policy discussions.
This historic move by the U.S. government represents a significant step towards addressing the high costs of prescription drugs, a long-standing issue in the American healthcare system. As the effects of these negotiations unfold, they may pave the way for further reforms in drug pricing and healthcare policy in the United States.