Weight-Loss Drug Shortages Spark Patient Anxiety and Treatment Challenges
Patients face anxiety and health setbacks as weight-loss drug shortages persist. Doctors and consumers grapple with inconsistent supply, raising concerns about long-term usage and equitable access to these medications.

The recent surge in popularity of weight-loss medications has led to unexpected challenges for patients and healthcare providers alike. Maez Waibel, a 29-year-old from Downingtown, Pennsylvania, experienced significant weight loss using these drugs but soon faced anxiety due to supply shortages. This situation highlights the complex issues surrounding the availability and use of GLP-1 receptor agonists, a class of drugs that includes Ozempic, Wegovy, Mounjaro, and Zepbound.
GLP-1 receptor agonists, first introduced with exenatide in 2005, have revolutionized weight loss and diabetes treatment. These medications mimic a naturally occurring hormone that reduces hunger and lowers blood sugar. However, their success has led to unprecedented demand, causing supply chain disruptions and leaving many patients in limbo.
The FDA reported in August 2024 that while Mounjaro, Ozempic, and Zepbound were available in all dosages, shortages of Wegovy persisted. This inconsistent supply has forced patients to adapt their treatment plans, often switching between medications or altering dosages. Some, like Waibel, have experienced weight regain during periods without access to their prescribed medication.
Healthcare professionals are grappling with these challenges as well. Diana Thiara, medical director at the University of California at San Francisco Weight Management Clinic, described the situation as "horrible," noting the difficulty in starting new patients on treatments when supply is unreliable. This unpredictability has led some patients to consider alternative options, such as bariatric surgery, which can result in 20-35% body weight loss for severely obese individuals.

The financial implications of these medications are significant. Without insurance, they can cost approximately $1,000 per month. This high price point has raised concerns about equitable access, as noted by Melanie R. Jay, co-director of the NYU Langone Comprehensive Program on Obesity. The global market for weight loss drugs is projected to reach $54 billion by 2030, underscoring the economic impact of these treatments.
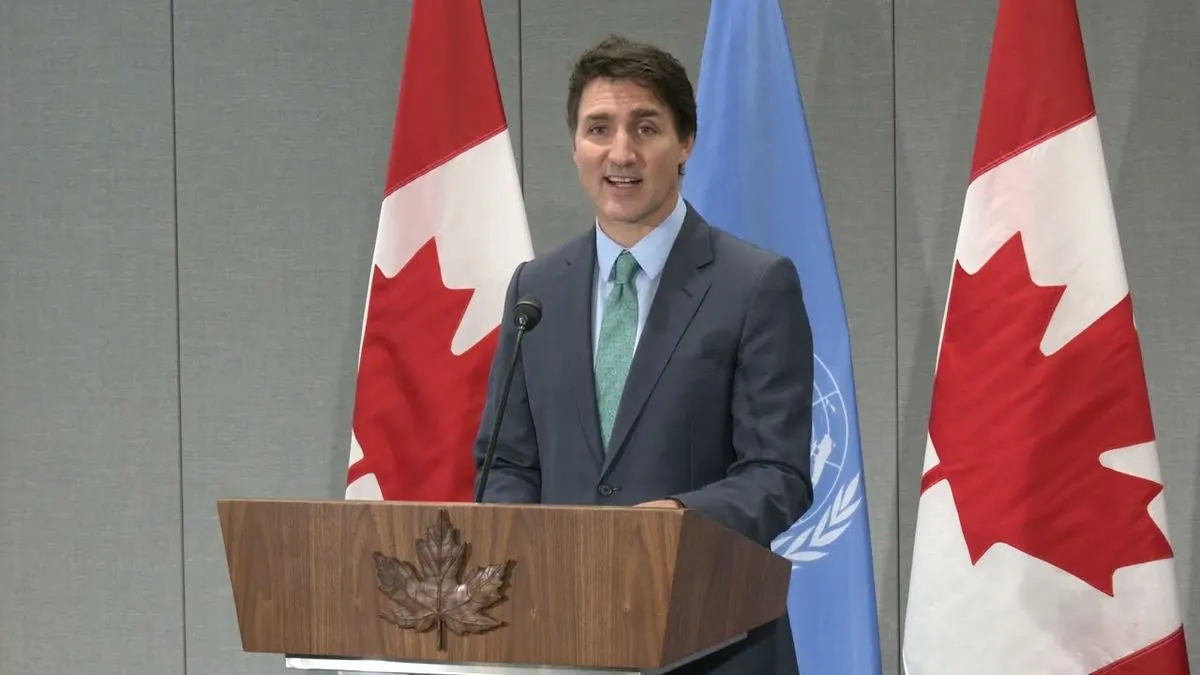
"The issue that we're discussing today is so important it impacts every aspect of our health-care system, the federal budget, private insurance."
The Senate held a hearing on September 24, 2024, to address the high prices of these drugs in the United States compared to other countries. This disparity in pricing has sparked debates about healthcare system reform and pharmaceutical company practices.
Long-term usage of these medications remains a topic of discussion among medical professionals. While they are approved as "forever" drugs, studies show that many patients discontinue use within the first year. A report by Blue Cross Blue Shield Association in May 2024 found that over 30% of patients stopped treatment after just four weeks.
Researchers are now exploring intermittent use of these drugs to address both patient needs and financial concerns. David E. Cummings, a professor of medicine at the University of Washington, noted that studies on shorter on-off intervals are underway, but results may take years to materialize.
As the obesity epidemic continues to affect approximately 42.4% of adults in the United States, the demand for effective treatments remains high. The US spends about $173 billion annually on obesity-related healthcare costs, emphasizing the need for accessible and sustainable solutions.
In conclusion, while GLP-1 receptor agonists offer promising results for weight loss and diabetes management, their widespread adoption has exposed weaknesses in the healthcare system. Patients like Waibel and others continue to navigate the challenges of inconsistent supply, financial barriers, and uncertain long-term effects. As research progresses and supply chains adapt, the hope is that these innovative treatments will become more readily available to those who need them most.